By Jessica Daniels
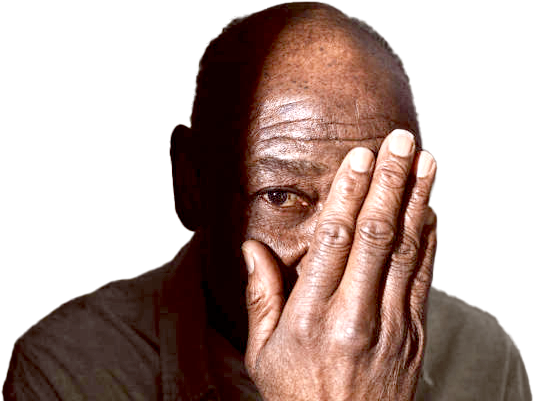
Most people have heard about glaucoma and cataracts, but there’s another eye disease that senior citizens should know about, especially those of European descent. This is macular degeneration, or damage to the macula, an ultrasensitive part of your retina that gives you sharp focus in the center of your vision. If you develop this condition, you may have trouble driving, reading, recognizing people, or other activities that require fine central vision. You may eventually experience major vision loss. Macular degeneration affects more than 1.75 million Americans and is the leading cause of legal blindness in older Americans. It’s important to know, though, that macular degeneration almost never causes complete blindness. In fact, most patients who have the disease can continue to live productive and independent lives.
There are two basic types of macular degeneration, known as “dry” and “wet.” About 90 percent of all cases are the dry sort, in which the macula has simply grown thin over the years. The dry form progresses very slowly and may never interfere with a person’s life. Many people simply notice that their vision fades a bit when they read. The wet form of macular degeneration is much more serious. In this case, abnormal blood vessels grow beneath the retina and start to leak, creating a pool of blood and other fluids that damage your retina and block your vision. Occasionally, a dry case can turn wet. If you have the dry form, see an ophthalmologist immediately if your vision suddenly worsens.
Macular degeneration, whether it’s the dry or wet form, typically begins with subtle changes in vision that can gradually worsen over time. In its early stages, the symptoms may be mild and easy to dismiss, but recognizing them early is crucial to preserving vision. Both types of macular degeneration affect the macula — the central part of the retina responsible for sharp, detailed vision — and share many of the same initial warning signs.
Here are some of the most common symptoms of Macular degeneration:
Blurry or Fuzzy Vision: One of the earliest signs is a general blurriness or fuzziness in your central vision, making it difficult to read, recognize faces, or drive.
Distorted Vision (Metamorphopsia): Straight lines may begin to appear wavy or bent. For example, sentences in a book may no longer line up properly, or the edges of buildings might look warped.
Dark or Empty Areas in Central Vision: You might notice blank or shadowy spots appearing in the center of your field of view. These areas may small and expand over time, making everyday tasks more challenging.
Difficulty with Color Perception or Contrast: Colors might appear faded or less vibrant, and distinguishing between shades can become harder, especially in low light.
Increased Sensitivity to Glare: Bright light may become uncomfortable, and you may notice halos or glare interfering with your vision, particularly while driving at night.
If you experience any of these symptoms, it’s important to schedule an appointment with an ophthalmologist as soon as possible. Early detection and intervention can help slow the progression of the disease and protect your remaining vision.
According to John Hopkins Medicine, there are two primary types of age-related macular degeneration have different causes:
Dry macular degeneration. This type is the most common. About 80% of those with AMD have the dry form. Its exact cause is unknown, although both genetic and environmental factors are thought to play a role. This happens as the light-sensitive cells in the macula slowly break down, generally one eye at a time. The loss of vision in this condition is usually slow and gradual. It is believed that the age-related damage of an important support membrane under the retina contributes to dry age-related macular degeneration.
Wet macular dgeneration. Though this type is less common, it usually leads to more severe vision loss in patients than dry AMD. It is the most common cause of severe loss of vision. Wet AMD happens when abnormal blood vessels start to grow beneath the retina. They leak fluid and blood — hence the name wet AMD — and can create a large blind spot in the center of the visual field.
Age is by far the biggest risk factor for macular degeneration, although some rare forms of the disease can strike at any age. The disease sometimes develops during a person’s forties or fifties, but it’s much more common in people over 60.
The disease is rare among nonwhites. Some experts believe that excess exposure to ultraviolet rays can cause macular degeneration. This risk has not been proven, but a lifetime of sun worship without eye protection will definitely increase your risk of cataracts.
Yes. Macular degeneration runs in families, so be on guard if your parents or siblings have the condition. It’s also more common in women, smokers, and people with light-colored eyes. Those with cardiovascular disease also appear to be at higher risk.
A simple at-home test can help you detect macular degeneration before symptoms set in. You’ll need a special card that features a grid of straight lines with a dot in the center. This card, called a Yannuzzi card, is available from your doctor, and any person older than 50 should have one. Here’s how you use it: With your face 14 inches away from the card, close one eye and look at the dot. (Many people age 50 and older will need to use reading glasses.) If you have macular degeneration, the lines may look wavy, discolored, or otherwise distorted.
Your ophthalmologist will have to look at your retina to confirm a case of macular degeneration. People with the dry form of the disease will have small, round marks called drusen on their macula. If you have the wet form, the ophthalmologist will be able to detect blood vessels growing under your retina.